Adenoidid refers to disorders of the adenoids, which are pequeñas soft tissues located in the upper back of the throat area behind the nose. The condition is frequently searched by people mainly because of symptoms like nasal obstruction or sleep disturbance in children. This article discusses everything about adenoidid starting from its causes to its management. Breathing problems among children are a common worry for many parents and adenoidid is one of the major contributing factors. It is a condition that doctors mainly see in infants and toddlers but it can also occur in adults. Gaining knowledge on adenoidid will enable one to notice the early signs and get the necessary treatment. Adenoids serve as the body’s first barrier against the entry of bacteria and viruses but when they become enlarged or bacteria infect them, they cause the person to be uncomfortable.
What Are Adenoids?
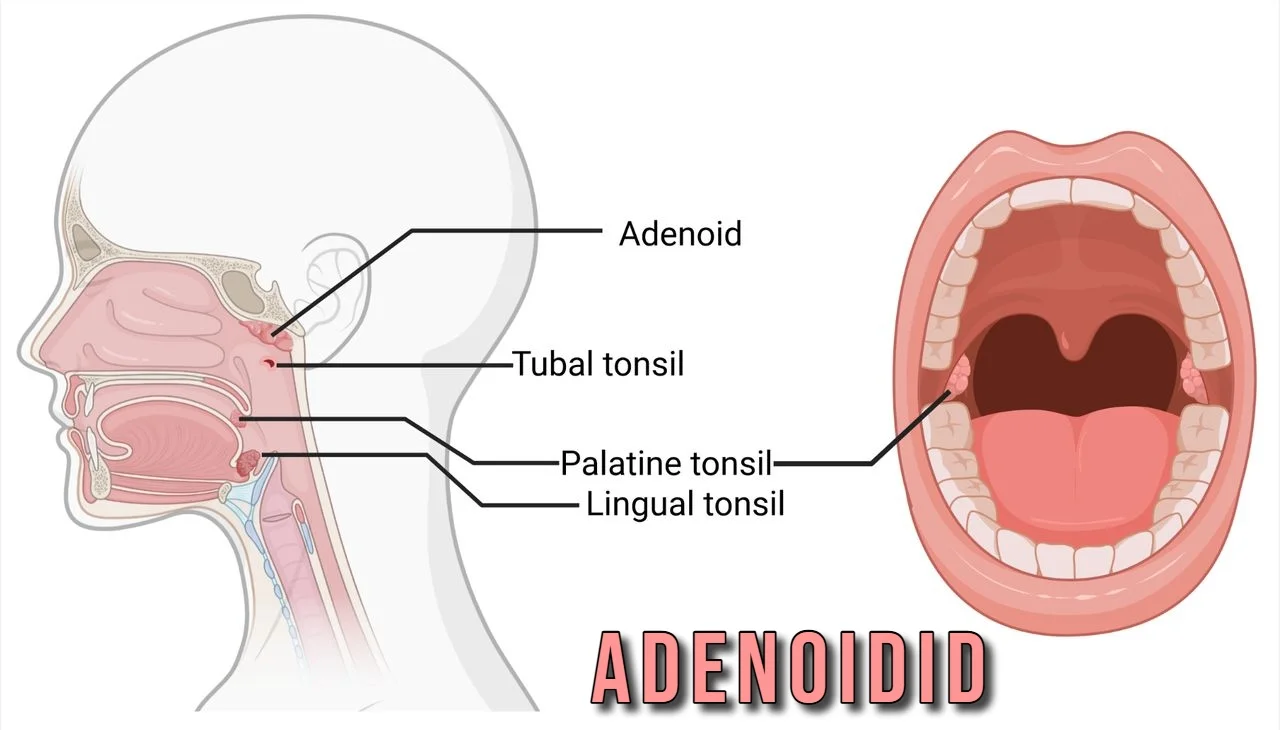
Adenoids are situated high in the pharynx, directly behind the nasal cavity. They constitute an element of the body’s immune system, composed of lymphatic tissue. In children, adenoids enlarge to capture pathogens entering via respiration. With advancing years, these tissues diminish, frequently disappearing by adolescence. Their placement within the nasopharynx renders them vital for the well-being of the upper respiratory tract. When functioning correctly, adenoids prevent lower spread of sicknesses. Issues arise if they become overly enlarged or frequently inflamed. This tissue resembles a soft mass, undetectable without instruments. Otolaryngologists examine them during check-ups. Understanding where adenoids reside assists in comprehending why particular signs surface with adenoiditis.
Adenoids belong to the Waldeyer’s ring, a circle of lymph tissues in the head and neck. This ring includes tonsils too. In early life, adenoids build immunity by sampling air for threats. They produce antibodies to fight off viruses and bacteria. Over time, other body parts take over this job, so adenoids shrink. In some cases, they stay large, leading to blockages. Research shows adenoids peak in size around ages three to seven. After that, natural reduction happens. If issues arise, it affects nearby areas like ears and sinuses. Parents notice changes in how kids breathe or speak. Regular check-ups catch these early.
Defining Adenoidid
Adenoidid describes swelling, infection, or overgrowth in the adenoids. It stems from repeated exposure to irritants or pathogens. Medical pros use terms like adenoiditis for inflammation specifically. Adenoidid covers a range of related conditions, focused on how adenoids impact daily life. In children, it shows up as blocked airways or frequent sickness. Adults rarely deal with it, but chronic cases occur. The term highlights functional problems over just anatomy. Sources note adenoidid as a way to group symptoms for easier discussion. Understanding this helps separate it from similar issues like tonsillitis. Treatment depends on severity and cause. Early awareness prevents complications.
Inflammation in adenoidid often links to immune responses gone overboard. The tissues react to allergens or microbes, causing enlargement. This blocks the Eustachian tubes, linking ears to throat. Resulting pressure changes lead to ear pain or infections. Speech can sound nasal due to poor airflow. Sleep gets disrupted from mouth breathing. Doctors diagnose through history and imaging. Adenoidid isn’t a standalone disease but a descriptor for adenoid troubles. It guides care plans. Families benefit from knowing signs to watch. Lifestyle tweaks sometimes ease mild cases. Severe ones might need surgery.
Common Causes of Adenoidid
Bacterial infections rank high among causes of adenoidid. Germs like Streptococcus or Haemophilus invade the tissues, sparking swelling. Kids in daycare pick these up easily from close contact. Viral culprits include rhinovirus from colds. Repeated episodes weaken defenses, making adenoids prone to chronic issues. Acid reflux irritates the area too, as stomach acids reach up. Allergies play a part, with pollen or dust causing ongoing inflammation. Environmental smoke or pollution worsens matters by irritating membranes. Genetic factors make some more susceptible. Identifying triggers allows targeted prevention. Doctors test for specific bacteria in stubborn cases.
Allergies trigger adenoidid by prompting histamine release, which swells tissues. Common allergens include pet dander, mold spores, or food items. In sensitive individuals, this leads to persistent nasal drip, feeding inflammation. Chronic sinusitis often pairs with it, creating a cycle. Immune system immaturity in young children heightens risk. Exposure to secondhand smoke damages protective linings. Poor diet lacking nutrients weakens overall resistance. Stress might indirectly contribute by lowering immunity. Pinpointing causes through allergy tests helps. Avoiding known irritants reduces flare-ups. Clean air at home supports recovery.
Infections from viruses like adenovirus or Epstein-Barr can initiate adenoidid. These spread through droplets in air or shared items. In crowded settings, outbreaks happen fast. Bacterial superinfections follow viral ones, complicating things. Gastroesophageal reflux sends acids to the nasopharynx, eroding tissues over time. Structural issues, like deviated septum, trap secretions and promote growth. Rarely, autoimmune conditions mimic adenoidid. Environmental toxins in urban areas add to the burden. Tracking patterns in symptoms reveals root causes. Lab work confirms infections. Addressing multiple factors improves outcomes.
Recognizing Symptoms of Adenoidid
Nasal blockage stands out as a key symptom of adenoidid. Airflow restriction forces mouth breathing, drying the throat. This leads to sore throats upon waking. Snoring occurs from partial obstruction during sleep. Kids might pause breathing briefly, hinting at apnea. Chronic runny nose with thick mucus is common. Ear fullness or popping sounds signal tube blockage. Hearing muffles, affecting school performance. Facial pain from sinus pressure adds discomfort. Bad breath results from trapped bacteria. Fatigue hits due to poor rest. Watching for these aids early intervention. Persistent symptoms warrant a doctor visit.
Speech changes mark adenoidid in many cases. Voices sound hyponasal, like talking with a plugged nose. This affects social interactions for children. Frequent coughing clears post-nasal drip. Swallowing feels off from swollen tissues. Headaches stem from sinus buildup. In severe instances, weight loss occurs from eating difficulties. Behavioral shifts, like irritability, reflect sleep loss. Fever accompanies acute infections. Monitoring duration helps gauge seriousness. Mild signs might resolve alone, but ongoing ones need checks. Parents track patterns to share with physicians. Simple home observations guide next steps.
Sleep disturbances define adenoidid’s impact. Noisy breathing interrupts rest cycles. Daytime sleepiness reduces focus. In kids, this mimics attention disorders. Restless nights lead to bedwetting sometimes. Growth slows if energy goes to breathing over development. Adults report concentration lapses at work. Tracking sleep quality reveals connections. Using apps or journals logs issues. Addressing symptoms restores normal patterns. Untreated, it strains heart and lungs long-term. Awareness prompts timely care. Families notice improvements post-treatment.
How Doctors Diagnose Adenoidid
Diagnosis begins with a detailed history of symptoms. Physicians ask about frequency of colds, allergies, or sleep issues. Physical exams include looking in the nose and throat. A flexible scope views adenoids directly without discomfort. X-rays or CT scans show size and inflammation if needed. Hearing tests check for fluid in ears. Swabs identify bacteria or viruses. Allergy skin tests pinpoint triggers. Blood work rules out other conditions. This approach ensures accurate identification. Follow-up visits monitor progress. Clear communication builds trust in the process.
Imaging plays a role in confirming adenoidid. Lateral neck X-rays measure adenoid size against airway space. Endoscopy offers real-time views, safe for most ages. In complex cases, MRI details soft tissues. These tools avoid guesswork. Specialists interpret results alongside symptoms. Ruling out polyps or tumors matters. Quick diagnosis prevents escalation. Families appreciate explanations during exams. Technology aids precision. Regular screenings in at-risk groups catch early changes. Lab tests support diagnosis by detecting infections. Cultures grow bacteria for targeted antibiotics. Viral panels use PCR for fast results. Allergy blood tests measure IgE levels. Complete blood counts show infection markers. These provide evidence-based insights. Combining methods paints a full picture. Physicians explain findings simply. This empowers informed decisions. Ongoing testing tracks treatment effects. Accuracy reduces unnecessary interventions.
Treatment Options for Adenoidid
Conservative treatments start with medications. Antibiotics tackle bacterial causes, prescribed after tests. Nasal steroids reduce swelling over weeks. Antihistamines control allergy symptoms. Decongestants offer short-term relief. Saline sprays clean passages naturally. Humidifiers moisten air, easing dryness. Lifestyle changes include elevating head for sleep. Avoiding irritants like smoke helps. Hydration thins mucus. These steps often suffice for mild cases. Monitoring ensures effectiveness. Adjustments come based on response. Patients see gradual improvement.Surgery becomes an option for persistent adenoidid. Adenoidectomy removes the tissues under anesthesia. It’s quick, with same-day discharge often. Recovery takes a week, with soft foods advised. Risks include bleeding, but rare. Benefits include better breathing and fewer infections. Combined with tonsillectomy if needed. Candidates show chronic symptoms despite meds. Post-op care prevents complications. Follow-ups confirm healing. Many report life-changing results. Weighing pros and cons guides choices.
Home remedies support medical treatments. Warm compresses soothe facial pain. Herbal teas calm throats. Probiotics boost gut health, aiding immunity. Essential oils in diffusers clear airways. Rest allows body repair. Diet rich in vitamins strengthens defenses. Exercise promotes circulation. These complement professional care. Consistency yields best outcomes. Tracking helps refine approaches. Families integrate them into routines. Safety comes first with natural methods.Alternative therapies offer added relief. Acupuncture targets energy flow for inflammation. Chiropractic adjustments improve drainage. Yoga poses enhance breathing. Massage loosens tight areas. These suit those seeking non-drug options. Evidence varies, so consult experts. Integrating with standard care maximizes benefits. Personal experiences guide selection. Research supports some for symptom management. Open discussions with doctors ensure compatibility.
Preventing Adenoidid
Good hygiene cuts infection risk. Hand washing removes germs. Vaccines protect against common viruses. Healthy diets fuel immunity. Fresh fruits and veggies provide antioxidants. Sleep routines strengthen resistance. Stress management through play or relaxation helps. Clean homes reduce dust. Air filters trap allergens. Regular exercise builds stamina. These habits form a strong base. Families adopt them early. Community efforts limit spread in schools. Awareness spreads through talks. Prevention saves time and worry.
Allergy control prevents adenoidid flares. Identifying triggers through tests allows avoidance. Medications keep reactions in check. Immunotherapy desensitizes over time. Pet-free zones limit exposure. Pollen alerts guide outdoor plans. Diet tweaks eliminate food sensitivities. These steps maintain clear airways. Monitoring weather aids preparation. Support groups share tips. Long-term commitment pays off. Health improves steadily.Environmental changes guard against adenoidid. Smoke-free spaces protect lungs. Ventilation clears indoor air. Green plants filter toxins. Avoiding harsh cleaners reduces irritation. Travel precautions include masks. These create safe surroundings. Community policies enforce clean standards. Education empowers choices. Benefits extend beyond adenoids. Overall wellness rises.
Adenoidid in Children Compared to Adults
Children face adenoidid more due to developing systems. Tissues grow actively, reacting strongly to threats. Daycare increases exposure. Symptoms disrupt learning and play. Growth delays possible if chronic. Parents spot changes in behavior. Early care shapes outcomes. Natural shrinkage eases issues by adolescence. Focus lies on supportive measures. Surgery resolves stubborn cases. Monitoring growth ensures timely action. Families find relief in progress.
Adults encounter adenoidid less often. Remaining tissues suggest chronic problems. Allergies or reflux dominate causes. Symptoms mimic sinus issues. Work impacts motivation. Diagnosis needs thorough checks. Treatments mirror children’s but consider lifestyles. Surgery rare but effective. Prevention emphasizes health maintenance. Awareness grows with age. Outcomes favor quick resolution.
Differences stem from anatomy. Kids’ adenoids block more easily. Adults rely on other defenses. Symptom tolerance varies. Children adapt but suffer long-term. Adults seek care faster. Tailored approaches respect age needs. Research highlights these gaps. Care evolves accordingly.
Living with Adenoidid
Daily management eases adenoidid effects. Routines include nasal care. Tools like neti pots flush sinuses. Breathing exercises train better habits. Support from groups connects experiences. Apps remind medication times. Adjustments at school or work accommodate needs. These build resilience. Positive mindsets aid coping. Progress inspires continuity. Health becomes priority.
Complications arise if ignored. Chronic infections spread. Hearing loss affects communication. Sleep apnea strains systems. Speech delays in kids hinder development. Prompt action averts these. Regular checks catch shifts. Education prevents escalation. Outcomes improve with vigilance.
Research advances understanding. Studies explore genetics. New meds target inflammation. Minimally invasive surgeries refine techniques. Vaccines reduce triggers. Future holds better prevention. Staying informed guides choices. Contributions to science help all.
Conclusion
Adenoidid involves adenoid troubles that affect breathing, sleep, and health, mainly in children. Causes range from infections to allergies, with symptoms like nasal blocks and snoring. Diagnosis uses exams and imaging, while treatments include meds or surgery. Prevention through hygiene and environment control keeps issues at bay. This knowledge equips families to handle adenoidid effectively, improving quality of life. Spotting signs early leads to better results. Consult professionals for personalized advice. Staying proactive ensures comfort and wellness.
FAQs on Adenoidid
What makes adenoidid different from tonsillitis?
Adenoidid focuses on nasal tissues, causing stuffy noses and ear issues. Tonsillitis hits throat glands, leading to swallow pain. Both stem from similar germs but affect distinct areas. Treatments overlap, like antibiotics, but surgery targets specific sites.
Can adenoidid go away without treatment?
Mild cases resolve as children grow and adenoids shrink. Infections clear with rest. Chronic ones need intervention to avoid complications. Watch symptoms closely.
When should surgery be considered for adenoidid?
If meds fail and symptoms persist, like repeated infections or apnea, removal helps. Doctors assess based on impact.
Are there risks with adenoid surgery?
Bleeding or infection occur rarely. Most recover smoothly. Discuss concerns with surgeons.
How does diet affect adenoidid?
Nutrient-rich foods boost immunity. Avoiding allergens prevents flares. Hydration aids mucus flow.